It is equally critical to ensure that healthcare providers are paid for their services in the healthcare sector as it is to provide care. Though medical professionals deal with patients, medical billing and collection look after the business aspect of the health care services. In this regard, the billing and collection process in medicine is probably the most important, as it deals with collecting dues from the patients and the insurance companies within an acceptable time frame.
As simple as it may look, the collection process in medical billing can be intricate, with several layers and many actors involved. Yet, it is a critical process to enable cash flow and stability in the finances of a healthcare practice. Therefore, let us examine the collection process regarding medical billing and the steps involved. The value of medical billing services in facilitating the process.
The Importance of the Collection Process in Medical Billing
In medical billing, collection involves a series of actions to obtain payments from patients and insurance payors after medical care has been rendered. This key aspect is crucial for any medical practice or hospital to ensure that medical care providers receive payment for the services they provide.
Without an effective collections process, healthcare organizations may face slow collections, rising accounts receivables, and, even worse, uncollectibles. The collection process in medical billing ideally contains these challenges, seeking to ensure a positive movement of payments and minimize the likelihood of claims being denied or written off. It also requires promptly contacting patients and insurance providers for any payments due and completing the relevant documentation.
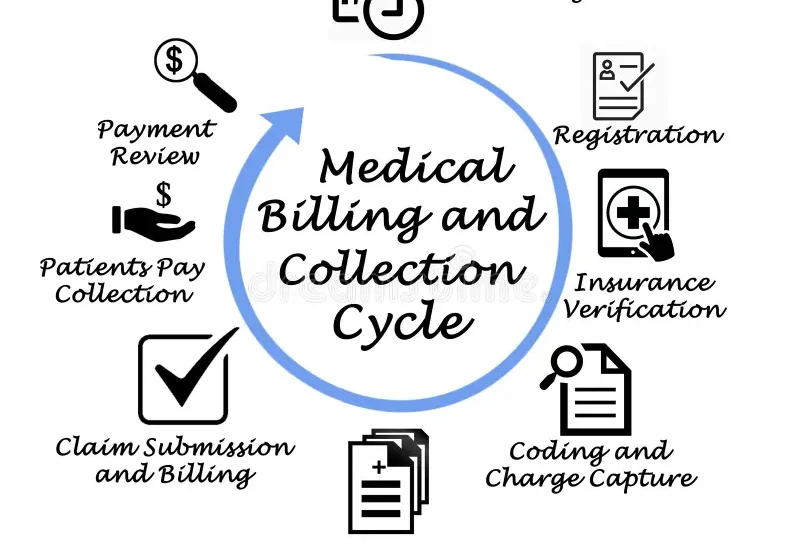
Stages of the Collection Process in Medical Billing
The collection process in medical billing typically follows several key stages, each requiring careful attention to detail and prompt action. Here’s a breakdown of the typical stages of collection process in medical billing:
Verification of Insurance Eligibility
It is important to check the patient’s insurance coverage before the commencement of any billing. Medical billing services usually start with verifying insurance information during service. This includes looking up the patient’s eligibility and checking the policy details and the range of coverage offered.
Insurance verification ensures that health payers receive claims accurately. Thus preventing potential challenges later in the process. This also helps the billing team inform the patients about the amount they need to clear. Thus minimizing shock during the bill clearance period.
Submitting the Initial Claim
The final step in providing care is to file the claim with the insurance company. Depending on the payer, this can be done electronically or with hard-copy claims. The claim also contains necessary codes such as diagnosis and procedure codes and relevant text. In this phase, accuracy is essential because attention to detail greatly affects business processes, such as reimbursements for medical claims. In medical billing collections management. One of the most important management steps is submitting a clean claim warranting prompt payment. Medical billing services incorporate the use of software and tools to simplify the process and, hence, minimize mistakes.
Claim Adjudication and Response
Adjudication for insurance is the process of processing or reviewing a claim. After that, the insurance decides to approve or reject the claim during adjudication. If the claim is accepted, they will pay the health care service provider directly. The insurance company explains why they did not accept the claim as unaffordable.
This stage is crucial for collection as it determines how much the insurer will reimburse and how much the patient will need to pay. Medical billing managing services closely monitor this stage and ensure that all necessary documents are provided to prevent unnecessary restrictions.
Patient Billing
The patient will be responsible for the remaining balance after payment from an insurance company. This may include co-pays, deductibles, or co-insurance. Only at this time are the patients sent a detailed statement of provided services and their costs. The payment is from insurance, and the patient owes the remaining balance.
Effective communication with the patient is essential at this stage. Sometimes, patients may have difficulty comprehending their balance, the services provided, and the bills their insurance can cover. This is where medical billing services step in and help teach the patients about their responsibilities and how they can pay. Such as through payment plans or payment assistance programs.
Follow-up on Outstanding Balances
Once the first invoice version is discharged to a patient, the other step in the collection process in medical billing domain is ensuring that she follows up on any outstanding balance. This could mean using reminders, making phone calls, and sending a second and third notice, among many others. Depending on the services offered and the importance of each service. Healthcare providers must efficiently track and collect all overdue payments in due time. If the patient is not cooperative and does not remit any payment, further measures must be undertaken by the billing services. Billing services may also engage patients in creative solutions such as payment plans or financial counseling. If all collection efforts fail, the company will standard practice to assign the uncollected debt to an external collection agency, which must be part of the resolution process.
Handling Denied or Underpaid Claims
Denial management is one of the most complex areas in the medical billing collection process. For example, if a claim is denied, it will be up to the medical billing services team to identify the cause of the denial and address the problem. This may require overturning the denial as part of the resolution process. It provides further evidence that fixing the mistake on the claim is necessary.
The performance of billing professionals will depend on their ability to appreciate the causes of denials and a plan to guard against them. Refused or underpaid claims are significant factors that strain a provider’s cash flow. Hence, it’s very important to have the mechanisms to detect and rectify the faults in the system quickly.
Escalating to Collections
The healthcare provider may refer the matter to collections if the patient’s account remains unpaid after all collection attempts. Medical billing services often engage third-party agencies to collect overdue amounts from patients who fail to pay their bills.
Collection agencies are proficient in recouping overdue amounts but tend to charge certain fees or take a percentage of the amount collected. While this can sometimes help to recover a portion of the money owed, it is often considered a last resort that may not be beneficial for maintaining patient relations.
Benefits of Outsourcing the Collection Process in Medical Billing
Outsourcing the collection process to expert medical billing services offers several advantages, including:
- Increased Productivity: The billing services have unique features and applications to facilitate the collection of debts while minimizing mistakes for fast payment.
- Knowledgeable Professionals: Most medical claim processing services have people skilled in coding and billing rules, and insurance companies make the filing of medical claims proficient and decrease the chances of rejections.
- Utilization of Resources: By using third parties for billing and collection, healthcare facilities can make more time available to themselves, which can be directed toward focusing on patient service.
- Enhanced Revenue: A well-addressed collection process in medical billing means that payments are received promptly, decreasing the number of pending debts and increasing the cash flow of the medical facility.
Conclusion
Collecting payments in medical billing is an essential part of managing the revenue cycle in the healthcare system. Each step – from checking the validity of insurance to the patient being billed and from pursuing any paid dues – is crucial in ensuring that the healthcare provider gets paid for the services offered. With these services, the practice can make more productive use of the doctors’ time. It lessens the chances of not receiving due collections through rejected claims. More importantly, it ensures that the practice collects all dues owed on time, enhancing its monetary status.
Given the tendency of healthcare billing and patient responsibility to become more complicated. A good and dependable collection process in medical billing is imperative for every healthcare provider. Whether done internally or engaged with third-party professionals. A good and efficient collection process in medical billing guarantees that patients and providers can fulfill their financial obligations.